Gdm ncp
Utilize this comprehensive nursing care plan and management guide to provide effective care for patients experiencing diabetes mellitus. Gain valuable insights on nursing assessmentinterventions, gdm ncp, goals, and nursing diagnosis specifically gdm ncp for diabetes mellitus in this guide. Diabetes mellitus DM is a chronic disease characterized by insufficient insulin production in the pancreas or when the body cannot efficiently use the insulin it produces. This leads to an increased concentration of glucose in the bloodstream hyperglycemia.
Watch More! Unlock the full videos with a FREE trial. Access More! View the full outline and transcript with a FREE trial. To guide nursing professionals in managing and supporting patients with Gestational Diabetes Mellitus GDM , focusing on understanding the condition, identifying risk factors and symptoms, and implementing effective interventions to manage blood glucose levels, prevent complications, and promote a healthy pregnancy and delivery. Gestational Diabetes Mellitus is a form of diabetes that develops during pregnancy.
Gdm ncp
Assess past 1. Maintain in 2. Assess and acquiring February 28, pregnancies. This acquiring normal monitor vital signs 2. Vital signs give you a baseline when a normal vital at 11 in clinical condition vital signs. It determines diet as which treatment moderated status with 4. Recognize her additional adverse condition and be protocols to follow, 3. Was the because of provide critical client able to consequences on knowledgeable her glucose information needed to understand the psychological about possible level make life-saving condition of her well-being andcomplications that quality of life. Adapt diet Meridian College. GDM is a changes to facilitate The results?
Self-monitoring of blood glucose should initially be performed at least four times daily: fasting and h postprandial, gdm ncp. Diet-specific to the individual is necessary to maintain normoglycemia and to obtained desired weight gain. Initial pharmacologic treatments for neuropathic pain in diabetes include gabapentinoids, serotonin- norepinephrine reuptake inhibitors SNRIs gdm ncp, tricyclic antidepressants TCAsand sodium channel blockers.
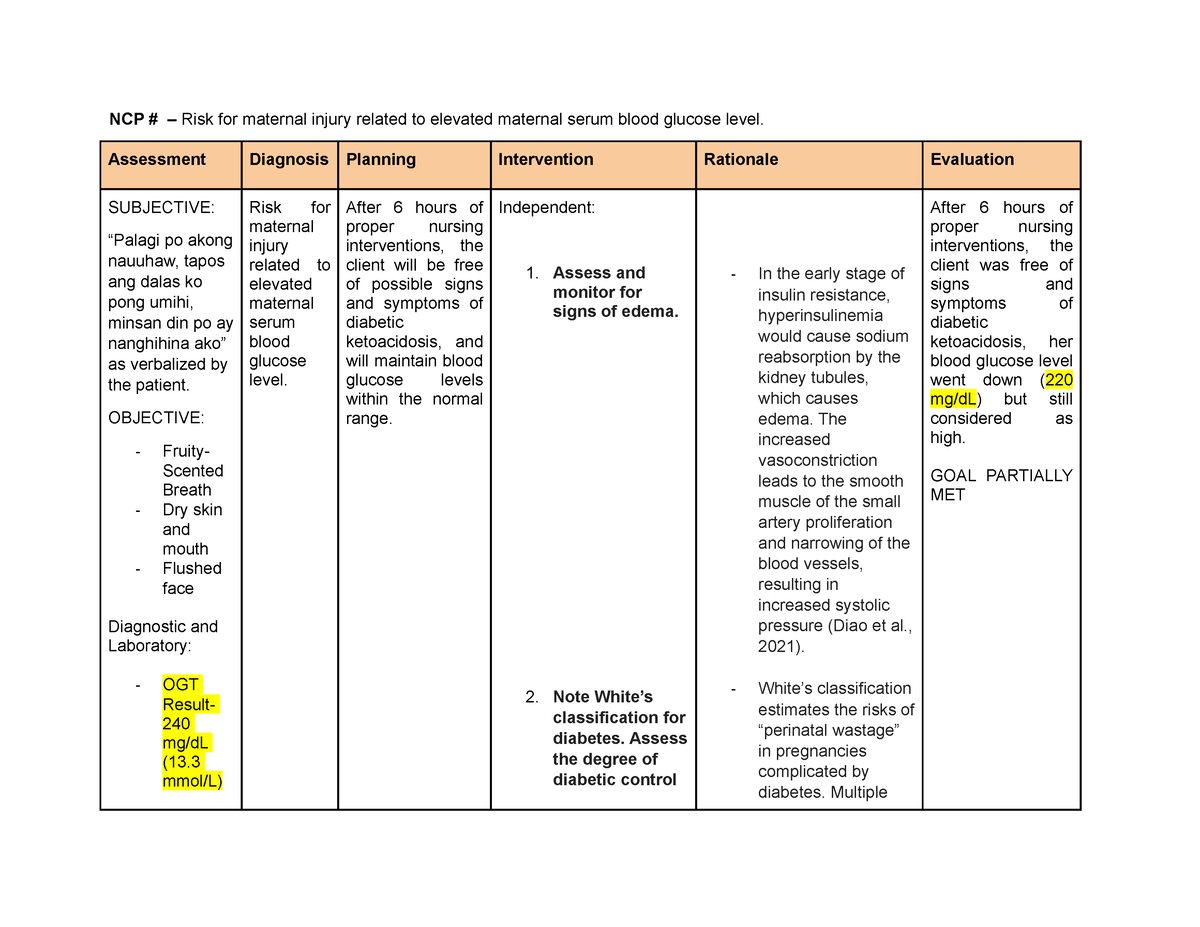
In true GDM, glucose usually returns to normal by six weeks postpartum , although women with GDM have an increased risk of developing type 2 diabetes mellitus later in life. The primary concern for any woman with this disorder is controlling the balance between insulin and blood glucose levels to prevent hyperglycemia or hypoglycemia. Women with gestational diabetes are at an increased risk of complications during pregnancy and delivery. The nursing care plan for gestational diabetes mellitus involves providing the client or couple with information regarding the disease condition, teaching insulin administration, achieving and maintaining normoglycemia, and evaluating the present client or fetal well-being. While nursing diagnoses serve as a framework for organizing care, their usefulness may vary in different clinical situations. In real-life clinical settings, it is important to note that the use of specific nursing diagnostic labels may not be as prominent or commonly utilized as other components of the care plan.
Federal government websites often end in. The site is secure. Gestational diabetes mellitus GDM poses well-established risks to both the mother and infant. Data suggest our current health services infrastructure loses patients in the postpartum gap between pregnancy-focused care and primary care. These strategies deserve future investigation to solidify a multi-level approach for identifying and preventing the continuum of diabetes. Gestational diabetes mellitus GDM is defined as glucose intolerance developed during pregnancy. The diagnosis of GDM bears associated short-term and long-term risks for both the infant and mother. The correlation between GDM and macrosomia, neonatal hypoglycemia, birth trauma, and subsequent overweight in the offspring has been well-established. The first step in long-term risk management of women with GDM is postpartum glucose tolerance testing. Women are additionally recommended to visit their primary care provider PCP within a year of delivery; PCPs may perform further metabolic testing, recommend pharmacologic therapy, and utilize lifestyle modalities to promote weight loss, which has been shown to reduce the onset of diabetes, as demonstrated in the Diabetes Prevention Program.
Gdm ncp
In true GDM, glucose usually returns to normal by six weeks postpartum , although women with GDM have an increased risk of developing type 2 diabetes mellitus later in life. The primary concern for any woman with this disorder is controlling the balance between insulin and blood glucose levels to prevent hyperglycemia or hypoglycemia. Women with gestational diabetes are at an increased risk of complications during pregnancy and delivery. The nursing care plan for gestational diabetes mellitus involves providing the client or couple with information regarding the disease condition, teaching insulin administration, achieving and maintaining normoglycemia, and evaluating the present client or fetal well-being. While nursing diagnoses serve as a framework for organizing care, their usefulness may vary in different clinical situations. In real-life clinical settings, it is important to note that the use of specific nursing diagnostic labels may not be as prominent or commonly utilized as other components of the care plan. Therapeutic interventions and nursing actions for patients with gestational diabetes mellitus GDM may include:.
T-shirt maradona
Providing snacks as needed helps maintain glucose levels and prevent hypoglycemic reactions in patients whose meals are delayed. Teach patients self-care techniques for maintaining eye health, including proper eye hygiene, protection from UV light, and recognition of warning signs requiring immediate medical attention. SMBG helps patients monitor their blood glucose levels and make necessary adjustments to insulin doses. Obesity or Overweight Advanced Maternal Age over 25 years old. Schedule for ophthalmologic examination during the first trimester for all clients and in second and third trimesters if clients are at class D, E, F. Early detection of UTI may prevent the occurrence of pyelonephritis, which can contribute to premature labor. By specifying three times per week with no more than two consecutive days without exercise, patients can maintain consistency in their exercise regimen, which contributes to better blood glucose control and overall fitness. Once you are finished, click the button below. The T-shaped plate model, especially for the main meals, is effective as a basic teaching tool to control portion size and plan meals more effectively. Ultrasonography is useful in confirming gestation dates and helps to evaluate intrauterine growth restriction IUGR , macrosomia, and excess amniotic fluid.
Gestational diabetes mellitus GDM is defined as any degree of glucose intolerance with onset or first recognition during pregnancy 1. The definition applies whether insulin or only diet modification is used for treatment and whether or not the condition persists after pregnancy. It does not exclude the possibility that unrecognized glucose intolerance may have antedated or begun concomitantly with the pregnancy.
Understanding the carbohydrate content of foods listed on nutrition labels allows patients to make informed choices and accurately determine the amount of medication needed, particularly for those who require premeal insulin. Review hematocrit and hemoglobin levels. Insufficient caloric intake is reflected by ketonuria, indicating a need for an increased intake of carbohydrates or additional snack in the dietary plan e. Pharmacotherapy aims to control blood glucose levels and prevent complications for both the mother and the developing baby. Question 11 Explanation:. Gestational diabetes can occur between the 16th and 28th week of pregnancy. Prevent complications related to GDM, such as preeclampsia, macrosomia, and birth injuries. Medication Administration: Administer or teach about the use of insulin or oral hypoglycemics if prescribed. Proper insertion and connection of the CGMS sensor and device are essential for accurate and reliable data collection. Lifestyle interventions, such as weight loss, adopting a Dietary Approaches to Stop Hypertension DASH eating pattern, reducing sodium intake, and increasing physical activity, are recommended. Non-Sulfonylurea Insulin Secretagogues [repaglinide Prandin , nateglinide Starlix ] Stimulates the pancreas to secrete insulin. Question 1. Long-acting insulins have an onset of one hour after administration, and have no peak action because insulin is released into the bloodstream at a relatively constant rate. Educate patients on pre-exercise carbohydrate snacks for insulin-treated individuals.

I am sorry, that I interrupt you, but you could not give more information.
I am sorry, that I interfere, but, in my opinion, there is other way of the decision of a question.