H5322 025 02 - hmopos
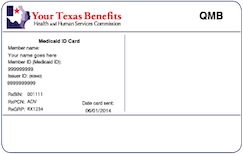
What is a dual special needs plan? If you can answer "yes" to the three questions below, there's a good chance you may qualify for this dual health plan. Search for doctors, hospitals, and specialists.
We're dedicated to improving your health and well-being. Members have access to specialized behavioral health services, which includes mental health and may include substance use treatment. Coverage services may vary based on eligibility. Search for providers, clinics and treatment centers. This search option is only available for desktop users. Note that you can download a list of covered drugs below. Search for drugs covered by our plan.
H5322 025 02 - hmopos
These SNP plans provide benefits beyond Original Medicare, such as transportation to medical appointments and routine vision exams. Members must have Medicaid to enroll. Health Maintenance Organization HMO plans use a network of contracted local physicians and hospitals to provide member care. Generally, members must use these care providers to receive benefits for covered services, except in emergencies. Some HMO plans do not require referrals for specialty care. Point of Service HMO-POS plans include all the features of HMO plans plus the ability to go outside the contracted network for certain health care services - typically at a higher cost. Some POS plans only cover out-of-network dental care. In addition, some POS plans do not require referrals for specialty care. Preferred Provider Organization PPO plans work with a network of contracted local physicians and hospitals, but also allows members the flexibility to seek covered services from outside of the contracted network, usually at a higher cost. Members do not need a referral for specialty care.
Find a Dentist.
.
We're dedicated to improving your health and well-being. Members have access to specialized behavioral health services, which includes mental health and may include substance use treatment. Coverage services may vary based on eligibility. Search for providers, clinics and treatment centers. This search option is only available for desktop users. Note that you can download a list of covered drugs below. Search for drugs covered by our plan.
H5322 025 02 - hmopos
Learn more about Texas Medicare Advantage plans like the one below and find a plan that offers the benefits you want at an affordable price. The following dental services are covered, though there may be provider network restrictions. See the plan Evidence of Coverage. The following vision services are covered, though there may be provider network restrictions. The following hearing services are covered, though there may be provider network restrictions.
Youtube true crime
Pill Icon. Care Icon. You must get your 1-month supply, as described in EOC, during the first 90 days of membership with the plan as a new member OR within the first 90 days of the calendar year if you are a continuing member and your drug has encountered a negative formulary change. Member Resources. Added Benefits Icon. Pill Bottle Icon. If we make a coverage decision and you are not satisfied with this decision, you can "appeal" the decision. Members must have Medicaid to enroll. For help scheduling an appointment, call the toll-free number on the back of your member ID card. Skip to main content.
What is a dual special needs plan? If you can answer "yes" to the three questions below, there's a good chance you may qualify for this dual health plan. Search for doctors, hospitals, and specialists.
Learn More. English Opens in a new tab PDF Mental Health Icon. This table shows you what your monthly plan premium will be if you get extra help. You can complete the CMR by phone or in person with a qualified health care provider. Skip to main content. You may also go to OptumRx to order and manage your prescription drugs online. When you get your flu shot, it is covered by the terms of your plan. Review the ANOC carefully to find out if your current drugs will be covered the same way in the upcoming year. Skip to main content. You must get your 1-month supply, as described in EOC, during the first 90 days of membership with the plan as a new member OR within the first 90 days of the calendar year if you are a continuing member and your drug has encountered a negative formulary change. Close modal. Search for doctors, hospitals, and specialists. Health Icon. Document Clipboard Icon.

The authoritative answer, it is tempting...
Yes, really. I agree with told all above. Let's discuss this question. Here or in PM.